
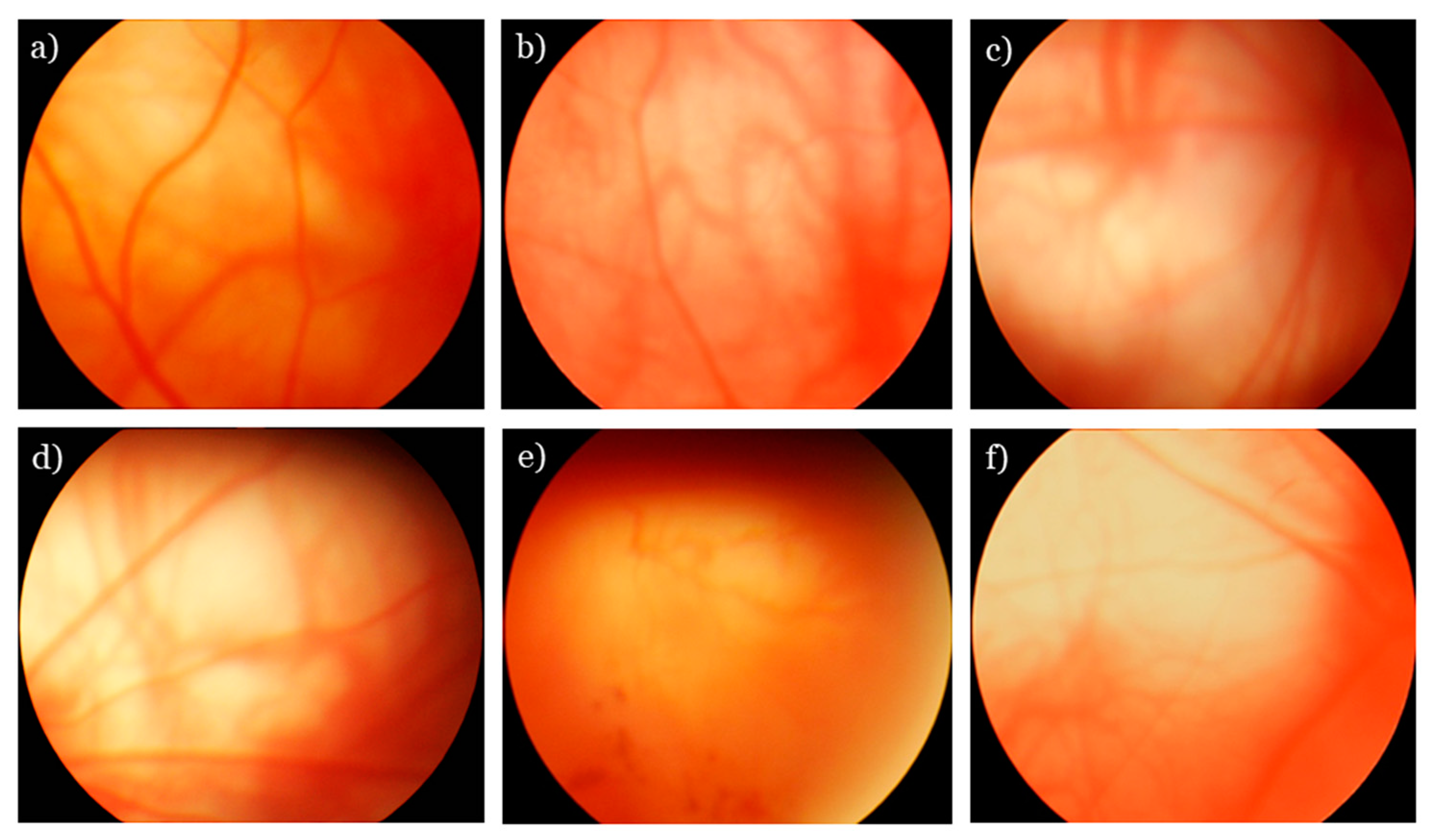
4-7,10,17 Pallor in PION is more likely to involve the temporal neuroretinal rim of the optic nerve, which correlates to central or paracentral visual field defects. It takes about two months for pallor to develop in a patient with AION, whereas pallor in PION may appear earlier, within three to eight weeks, although it typically becomes evident in the six- to eight-week range. 7 In the context of ION, it is important to observe the optic nerve appearance for edema upon acute onset of symptoms to rule out posterior vs. Several cases show blurred vision or loss of vision as early as day one to day five post-op. PION can present with acute vision loss post-surgically, during recovery from anesthesia. Congenitally small optic nerve cupping “disc at risk.”.Altitudinal or inferior nasal VF defects.Presence of optic disc edema initially.Optic atrophy develops nearly two months later.Commonly associated with hypotension and hemodilution.Optic nerve pallor develops on temporal neuroretinal rim.Optic atrophy develops acutely within three to eight weeks.1,4-6,11,12,14 (For a breakdown of factors in cases of both types of ischemic optic neuropathy, see “Signs and Symptoms of PION vs. With an acute presentation, the first can be readily distinguished from the other based upon the presence of disc swelling in the AION and absence of disc edema in PION. Optic atrophy develops after either anterior (AION) or posterior ischemic optic neuropathy (PION). 7,10,21 The posterior portion of the optic nerve extends from the lamina cribrosa to the optic foramen within the orbit. PO-ION typically involves the posterior optic nerve. It is considered a rare condition however, its incidence is rising due to the increased frequency of surgeries that predispose patients to PO-ION. PO-ION should be considered in cases when no other cause of ION can be determined. PO-ION in coronary artery bypass graft surgery is fairly rare however, it has shown an increase in frequency from 0.06% to 0.113% between the years 19. 5 A population-based study of vision loss after spine surgery showed an incidence of 0.006% cases of ION associated with spine surgery. 1,3,5-8,11,12,14-20Ī recent study showed that the incidence of symptomatic perioperative vision loss related to ION was 0.013%. Risk of PO-ION is increased by a number of conditions, including perioperative anemia, hypotension and direct pressure on the globe-and pre-existing systemic vascular conditions, such as hypertension and heart disease, are factors as well. Common procedures associated with PO-ION include coronary artery bypass surgery, spine surgery and radial neck dissection surgery. ION is the most common cause of postoperative vision loss. 1-4 The general term “perioperative vision loss” describes various subtypes of vision changes that occur during or after surgery, including ischemic optic neuropathy, cortical vision loss and/or vascular occlusions. PO-ION may occur in patients with predisposing systemic risk factors, such as a surgical complication. Although still considered rare, its incidence is increasing along with the frequency of surgeries at risk for with prolonged surgical times, risks for high volume blood loss, perioperative anemia and hypotension. Perioperative ischemic optic neuropathy (PO-ION) should be considered in cases where no other causes for ION are found.


 0 kommentar(er)
0 kommentar(er)
